Corneal thickness is a key factor at all stages of a refractive correction.1 The volume of tissue removal determines the refractive change2, the remaining cornea should at the same time affer enough stability.3 Ablations deeper than planned may lead to overcorrections and inadequate residual corneal thickness increases the risk of postoperative keratectasia.4 Ultrasound is the most common method of measuring corneal thickness. Newer methods based on Scheimpflug imaging6 and optical coherence tomography also allow the measurement of corneal pachymetry.
Optical coherence pachymetry has been recently introduced into clinical practice and this system is integrated in the SCHWIND AMARIS. This technique allows noncontact continuous monitoring of corneal thickness. The principle is based on low coherence interferometry, which detects very fine structures in the eye.
More than 100 eyes
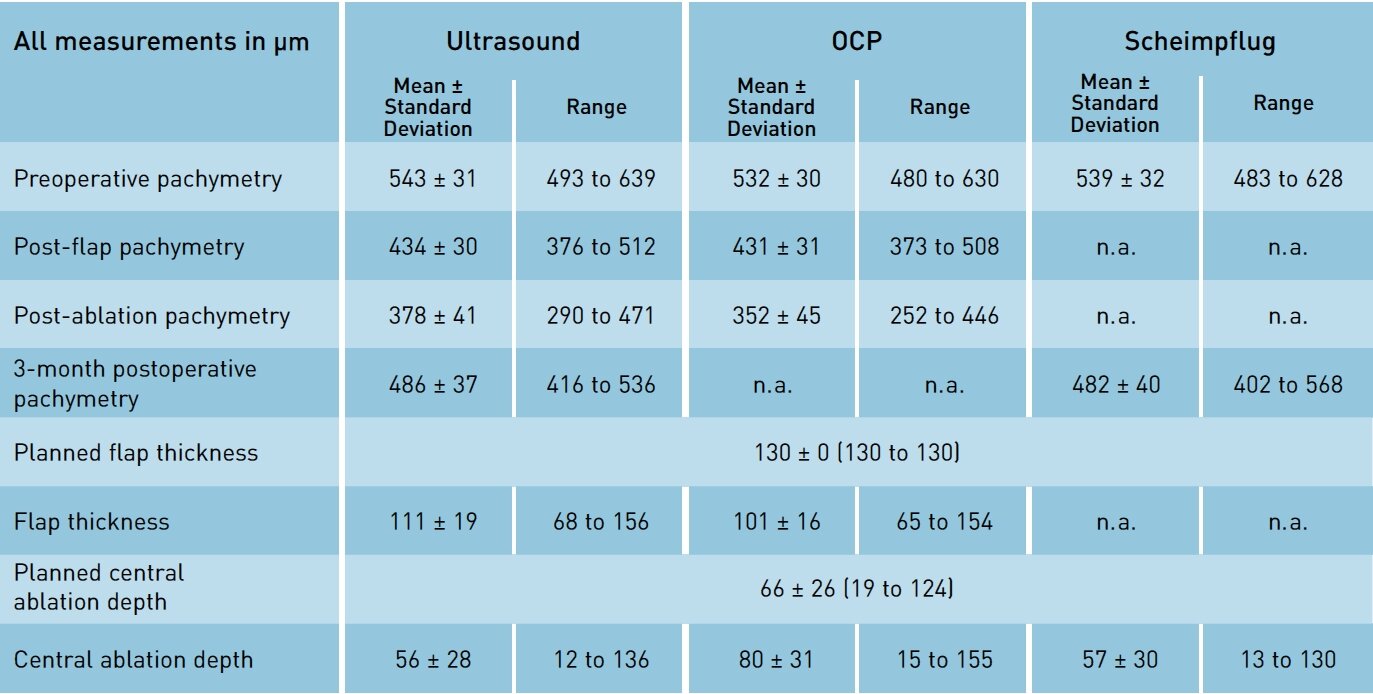
In a clinical study at the Muscat Eye Laser Center, Oman, with more than 100 eyes, corneal pachymetry was measured before and during the entire laser treatment. Preoperative pachymetry measurements correlated well for the three measurement techniques investigated in this study. There was fair correlation between ultrasound and OCP flap thickness measurements; however the OCP measured statistically significantly thinner flaps. Using the central ablation depth displayed on the laser screen as the reference measurement, there was very good correlation of central ablation depth for ultrasound, Scheimpflug, and Optical Coherence measurements. Correlation to the calculated central ablation depth was highest for OCP (mean deviation of +13 μm). The Scheimpflug measurement also showed good correlation (mean deviation of -9 μm) followed by ultrasound (mean deviation of -10 μm).
Continuous measurement
Comparing pachymetry deviations with the deviation in refractive results, there was no correlation for Scheimpflug, a borderline correlation for ultrasound and significant correlation for OCP. A highly significant correlation between the corneal pachymetry changes and the planned central ablation depth were found for all 3 techniques. The best correlation was with OCP, followed by Scheimpflug, and ultrasound. Thereby the OCP-measured ablation was statistically significantly deeper than the other two methods.
Unlike the other two methods, OCP provides continuous measurement during the laser ablation and gives information about potential corneal dehydration that increases the volume of tissue ablated. This dehydration effect may be transient and can only be detected with continuous monitoring. Continuous monitoring of the effect of corneal dehydration ensures that adequate residual stromal bed thickness remains after ablation in order to maintain the biomechanical integrity of the cornea.
The advantage of noncontact measurements is that they reduce the chance of infection. From the practical perspective, OCP is the best method of the three to continually monitor corneal pachymetry. The deviation between planned and actual central ablation depth could possibly point to inference of under- or overcorrection during laser treatment.
Encouraging findings
In the study, OCP showed encouraging findings in the prognosis of refractive results. Online OCP allowed the clinical evaluation of intraoperative ablation parameters during refractive surgery. Further studies are required to assess the active control of excimer laser ablation from continuous monitoring, which may improve laser algorithms and nomograms. Present study demonstrates that pachymetric measurements can be effectively used for monitoring and analyzing corneal laser refractive surgeries, helping to circumvent biomechanical weakening of the cornea. Optical coherence pachymetry is valuable to intraoperatively assess central corneal changes, flap thickness and residual stromal thickness.
1 Wang Z, Chen J, Yang B. Posterior corneal surface topographic changes after laser in situ keratomi-leusis are related to residual corneal bed thickness. Ophthalmology; 1999; 106: 406-9
2 Blaker JW, Hersh PS. Theoretical and clinical effect of preoperative corneal curvature on excimer laser photorefractive keratectomy for myopia. J Refract Corneal Surg; 1994; 10: 571-4
3 Roberts C. The cornea is not a piece of plastic. J Refract Surg; 2000; 16: 407-13
4 Binder PS. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg; 2007; 33: 1530-8
5 Salz JJ, Azen SP, Berstein J, Caroline P, Villasenor RA, Schanzlin DJ. Evaluation and comparison of sources of variability in the measurement of corneal thickness with ultrasonic and optical pachymeters. Ophthalmic Surg; 1983; 14: 750-4
6 O’Donnell C, Maldonado-Codina C. Agreement and repeatability of central thickness measurement in normal corneas using ultrasound pachymetry and the OCULUS Pentacam. Cornea; 2005; 24: 920-4
7 Wirbelauer C, Pham DT. Intraoperative optical coherence pachymetry during laser in situ keratomi-leusis-first clinical experience. J Refract Surg; 2003; 19: 372-7