Introduction
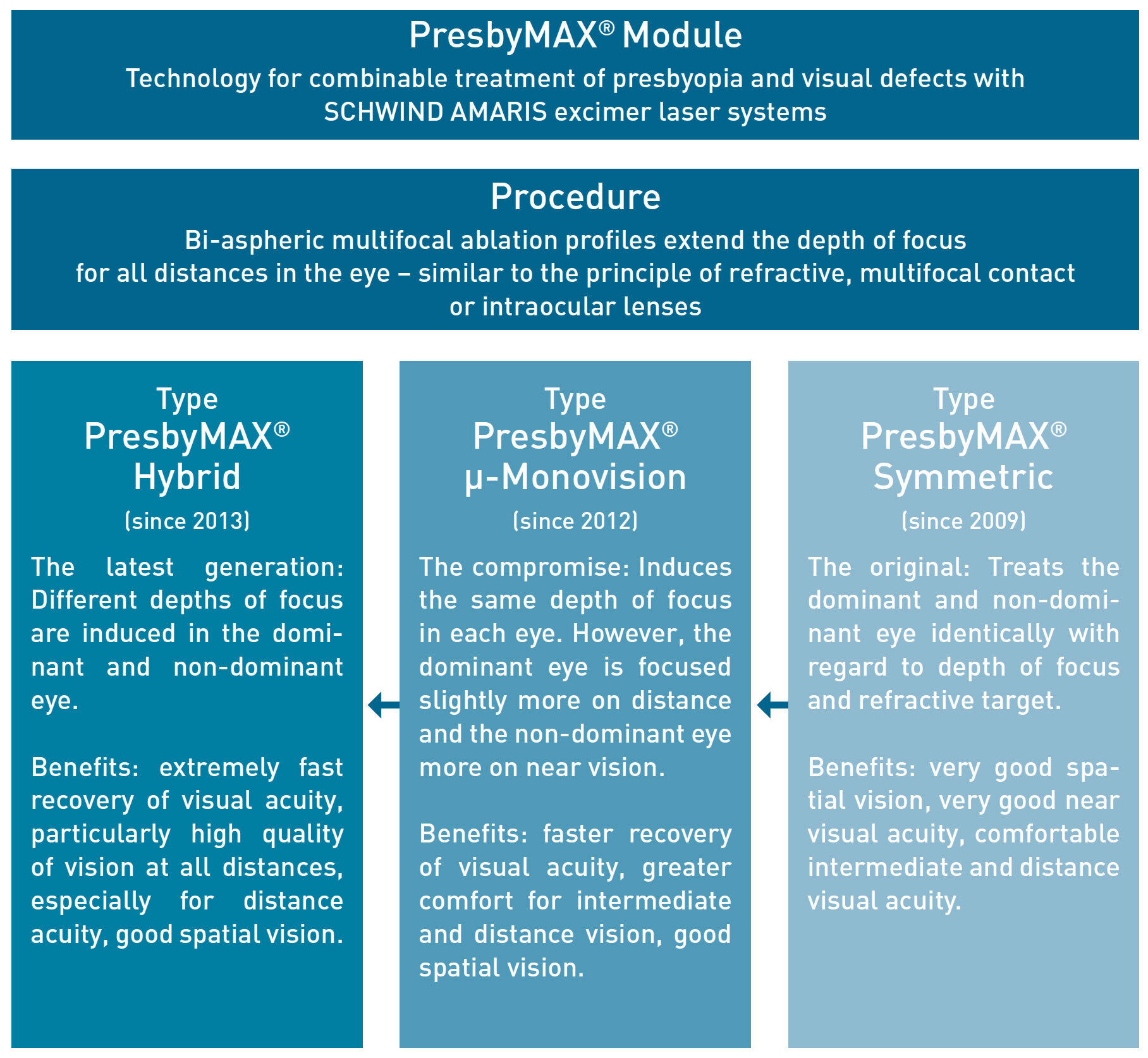
Since its market launch in 2009, the PresbyMAX procedure has become established as state-of-the-art technology for treating presbyopic patients. Up to now, more than 11,000 treatments worldwide have been successfully performed using this method. PresbyMAX Hybrid is the latest generation for the treatment of presbyopia by SCHWIND, providing an advanced approach built upon the foundations of PresbyMAX Symmetric and PresbyMAX µ-Monovision.
PresbyMAX Hybrid provides a different depth of focus for the distance and near eye. Apart from that, it offers all of the benefits and unique features of the tried and tested PresbyMAX technology. Altogether, a good binocular and spatial vision is provided. At far the same time, a particularly high quality of distance vision is achieved in the shortest recovery time.
Results
Visual Outcomes
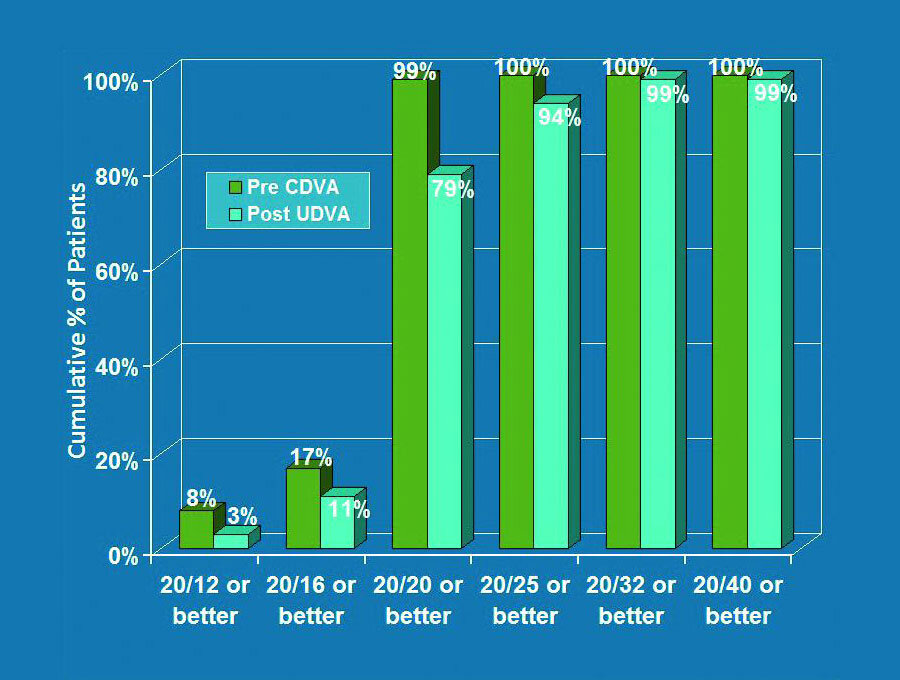
According to figure 1a (page 1) 94 % of 186 patients achieved an uncorrected distance visual acuity (UDVA) of 20/25 or better (0.1 logMAR or better) postoperatively.
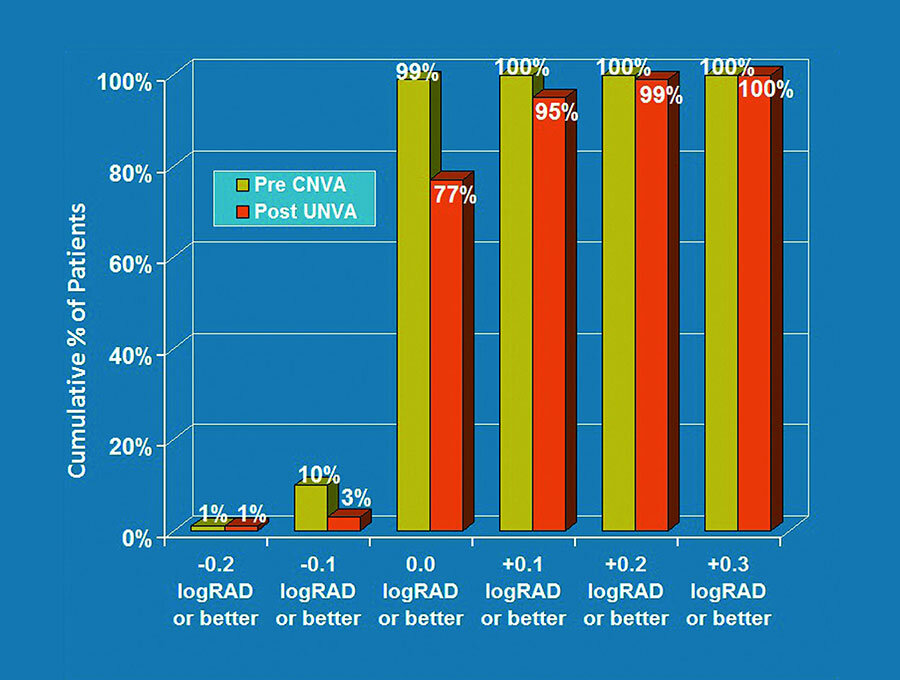
Figure 1b shows that postoperatively 95 % achieved an uncorrected near reading acuity (UNVA) of 0.1 logRAD or better (J2 or better).
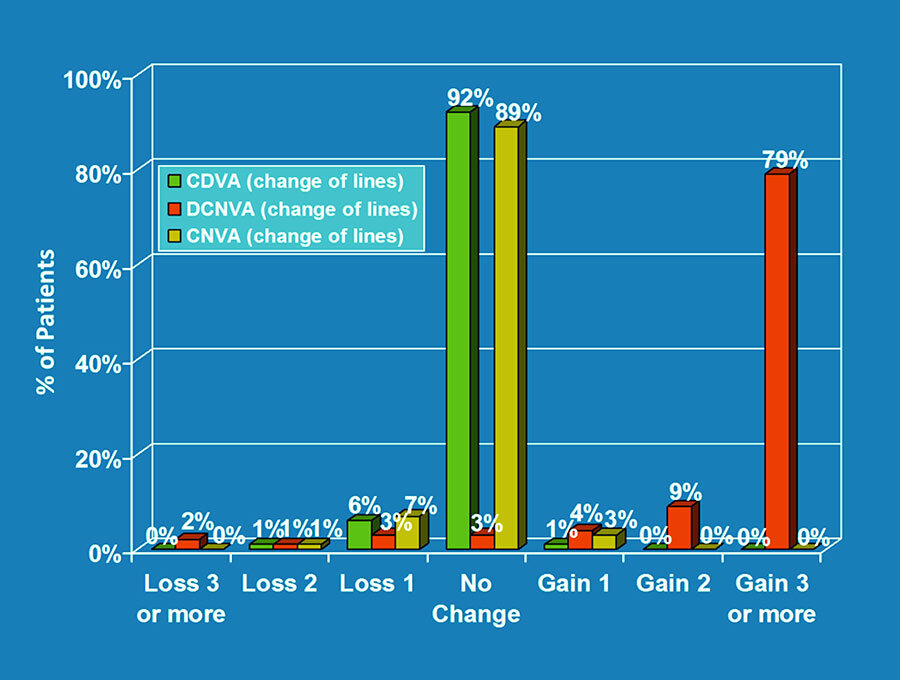
Figure 2 displays that 79 % of patients gained three or more Snellen lines in distance corrected near visual acuity (DCNVA), resulting from the multifocality created on the cornea. In more than 90 % of patients, the corrected distance visual acuity (CDVA) and the corrected near visual acuity (CNVA) remained unchanged or even showed a gain of one line.
Please notice that postoperative CDVA was always 20/25 or better.
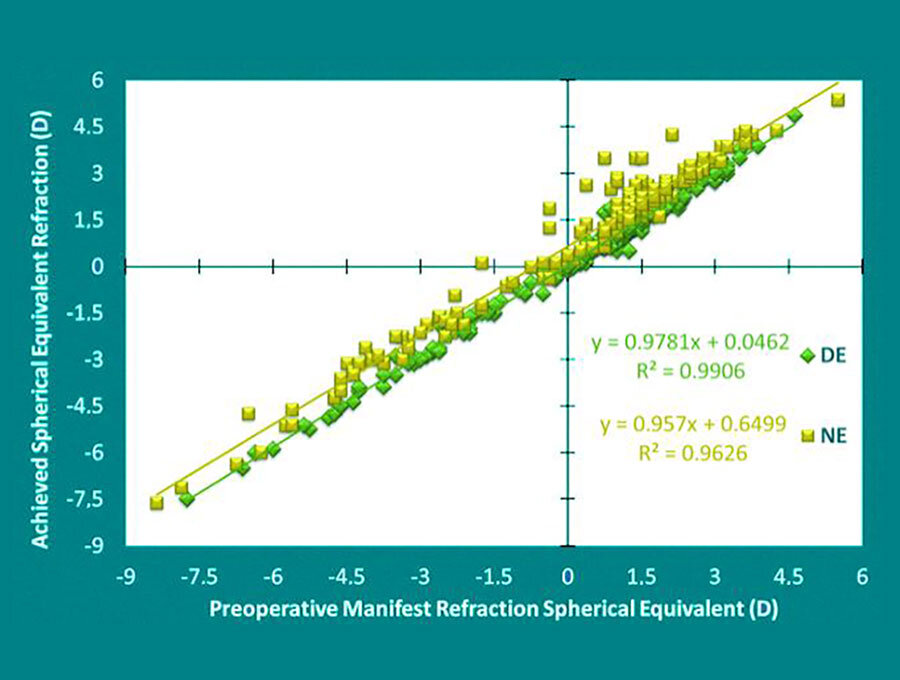
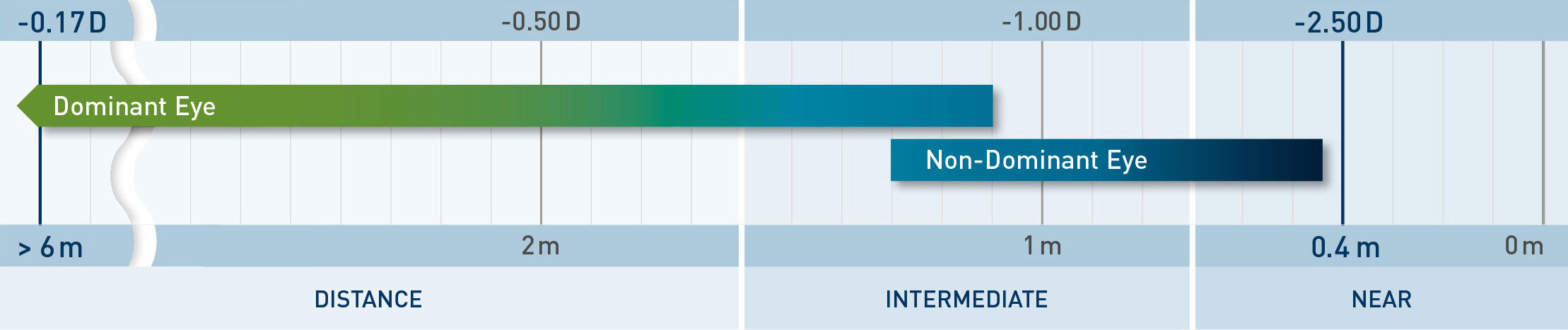
As presented in figure 3, the slopes of the distance and near eye show that the intended refractive target value was obtained with an average of 0.6 D anisometropia six months postoperatively.
Visual Outcomes
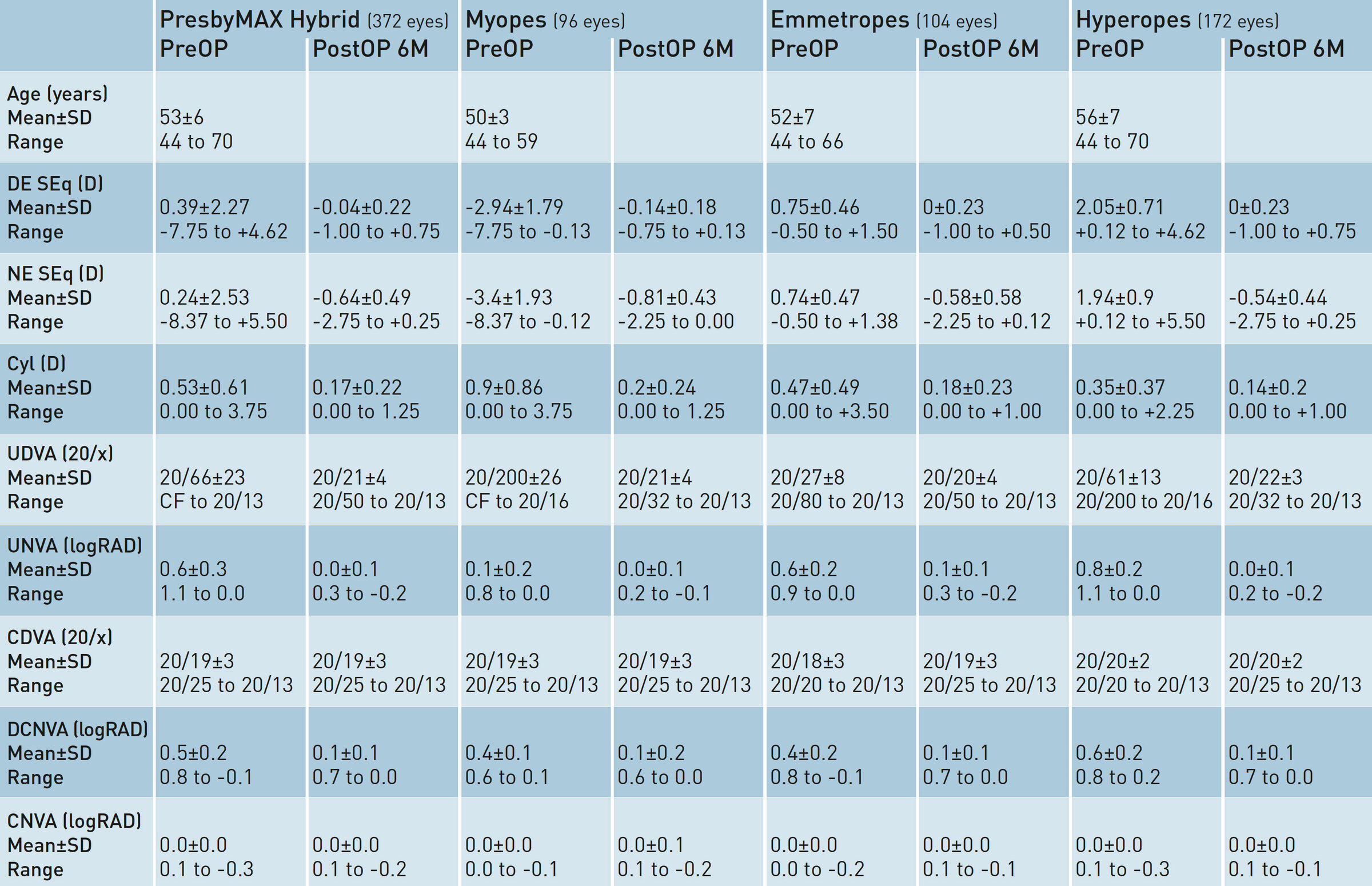
Table 1 presents the postoperative refractive and visual outcomes, stratified per refraction groups and overall outcome. It displays that the three individual groups (myopes: both principal meridians ≤ 0.0 D; emmetropes: SEq > 0.0 D and ≤ 1.0 D and Ast ≤ 1.0 D; hyperopes: SEq > 1.0 D or SEq > 0.0 D and Ast > 1.0 D) do not show significant differences compared to the total volume, i.e. a successful treatment with PresbyMAX Hybrid is independent of the kind of preoperative visual deficiency. Six months after the treatment, the target values for the distance and near eye are well achieved – in paticular in the myopic group.
Refractive Outcomes
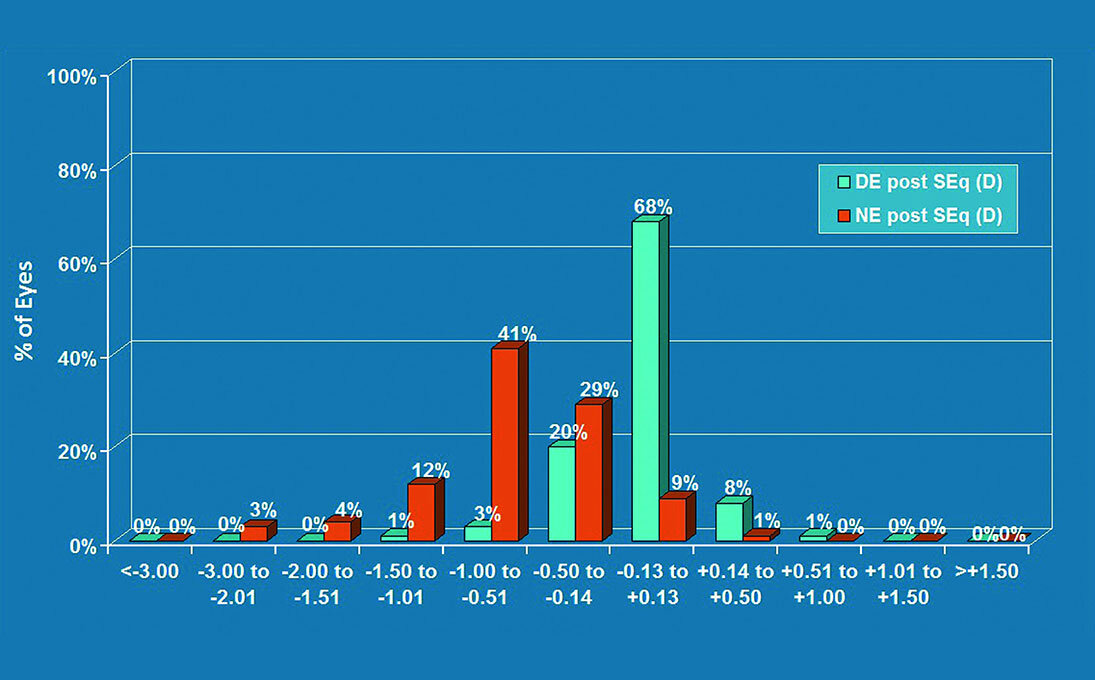
Predictability of the target refraction was also very good. After six months, 96 % of treated distance eyes were in the range of ±0.5 D SEq. 53 % of treated near eyes were in the range of -0.51 D to -1.5 D SEq, in combination with corneal multifocality providing very good reading abilities (figure 4a).
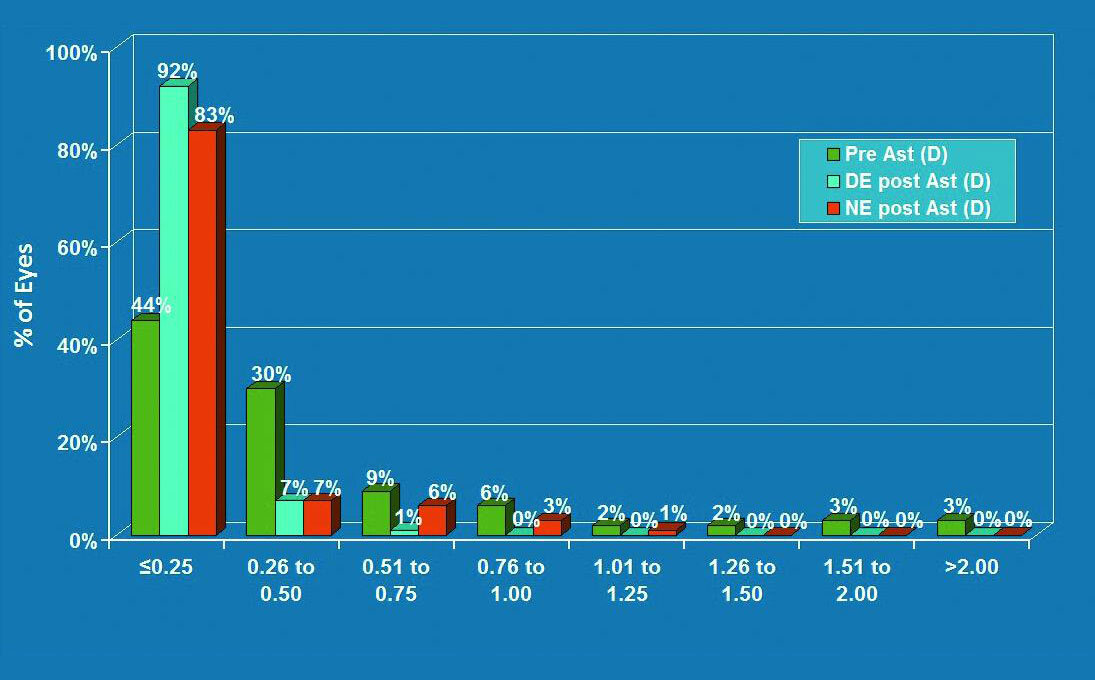
Figure 4b shows that after six months, 99 % of treated distance eyes and 90 % of treated near eyes were in the range of 0.5 D astigmatism; even reduced to 0.25 D or less in the majority of cases (preoperatively 44 % compared to postoperatively 92 % for the distance eye and 83 % for the near eye).
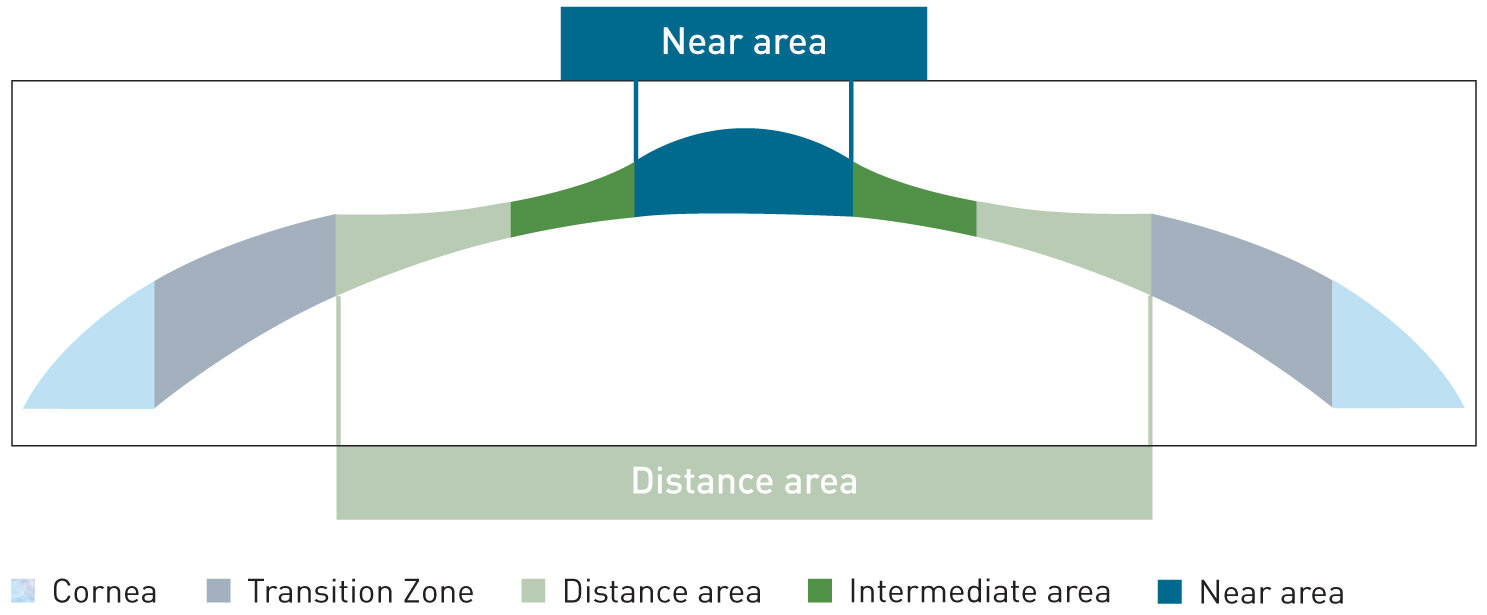
Figure 5 illustrates the range of vision at all distances that PresbyMAX Hybrid typically covers for the distance and the near eye, with aim of keeping binocular vision and stereopsis.
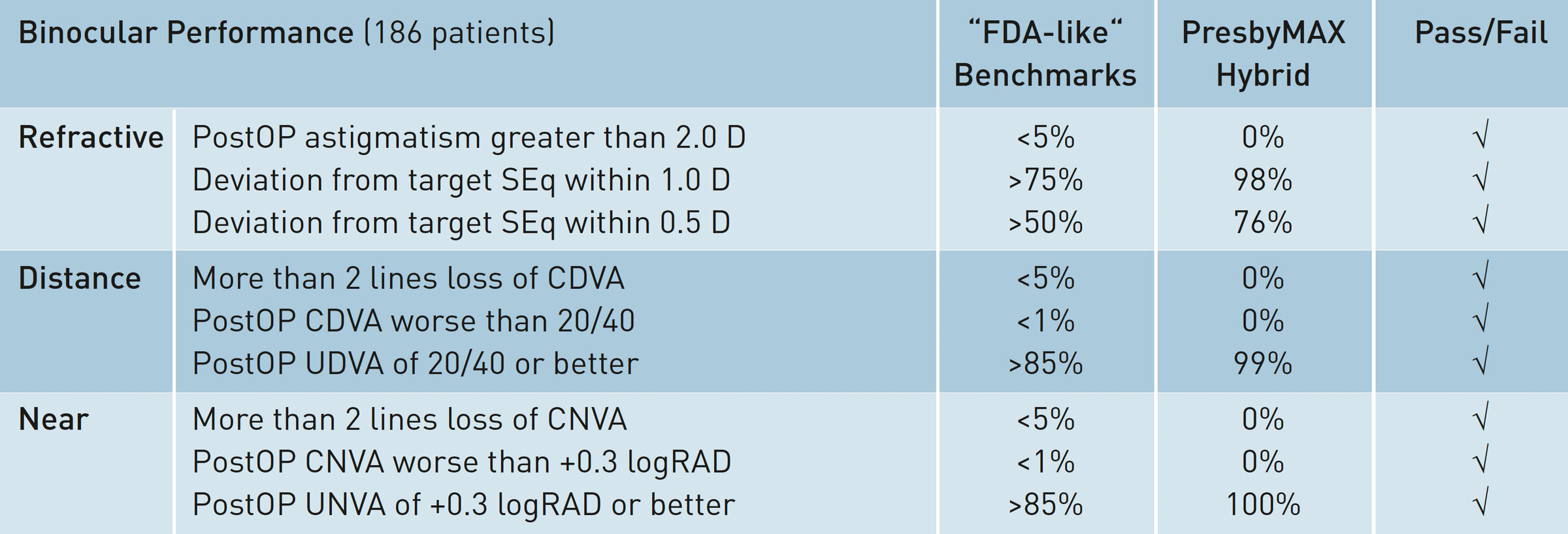
The PresbyMAX Hybrid study including 186 patients shows that the performance of the latest SCHWIND technology for treating presbyopia is significantly better compared to FDA-like benchmarks extended for near vision (table 2).
Summary
The six-month outcomes show that a high visual performance is achieved in both far and near distance. Preoperatively, 99 % of patients demonstrated a best corrected distance visual acuity of 20/20 or better. Six months after the treatment, 79 % of patients reached an uncorrected distance visual acuity of 20/20 or better.
Preoperatively, all patients showed a best corrected near visual acuity of 0.1 logRAD (J2) or better. At six months 95 % of patients achieved an uncorrected near visual acuity of 0.1 logRAD (J2) or better.
Impressive 79 % of patients gained three or more lines of distance corrected near visual acuity. The combination of multifocality and a negative defocus in the near eye provide an excellent reading vision without glasses in usual day-to-day situations.
Additionally, higher rates of patient satisfaction – even in demanding patients – were achieved with PresbyMAX Hybrid compared to earlier PresbyMAX approaches.
Conclusion
PresbyMAX Hybrid maximises functional vision at all distances, minimising detrimental effects in distance vision. At six months, results are significantly better compared to six-month results with PresbyMAX Symmetric (see SCHWIND study 2010). However, careful patient selection still plays an integral role in achieving high patient satisfaction. PresbyMAX Hybrid is currently the most frequently used technique within the SCHWIND portfolio for treating presbyopia.