The goal of refractive surgery in eyes that have not undergone any ocular surgery is to achieve post-operative uncorrected distance acuity (UDVA) that equals the preoperative corrected distance visual quality (CDVA). Hyperopic laser in situ keratomileusis (LASIK) has been shown to induce higher order aberrations (HOA)2 at a rate that is higher per corrected diopter than a similar group of myopic eyes3. Due to this reason, the magnitude of hyperopic corrections is generally less compared to myopic corrections (up to +6 or +7D, compared to -12 to -14D).
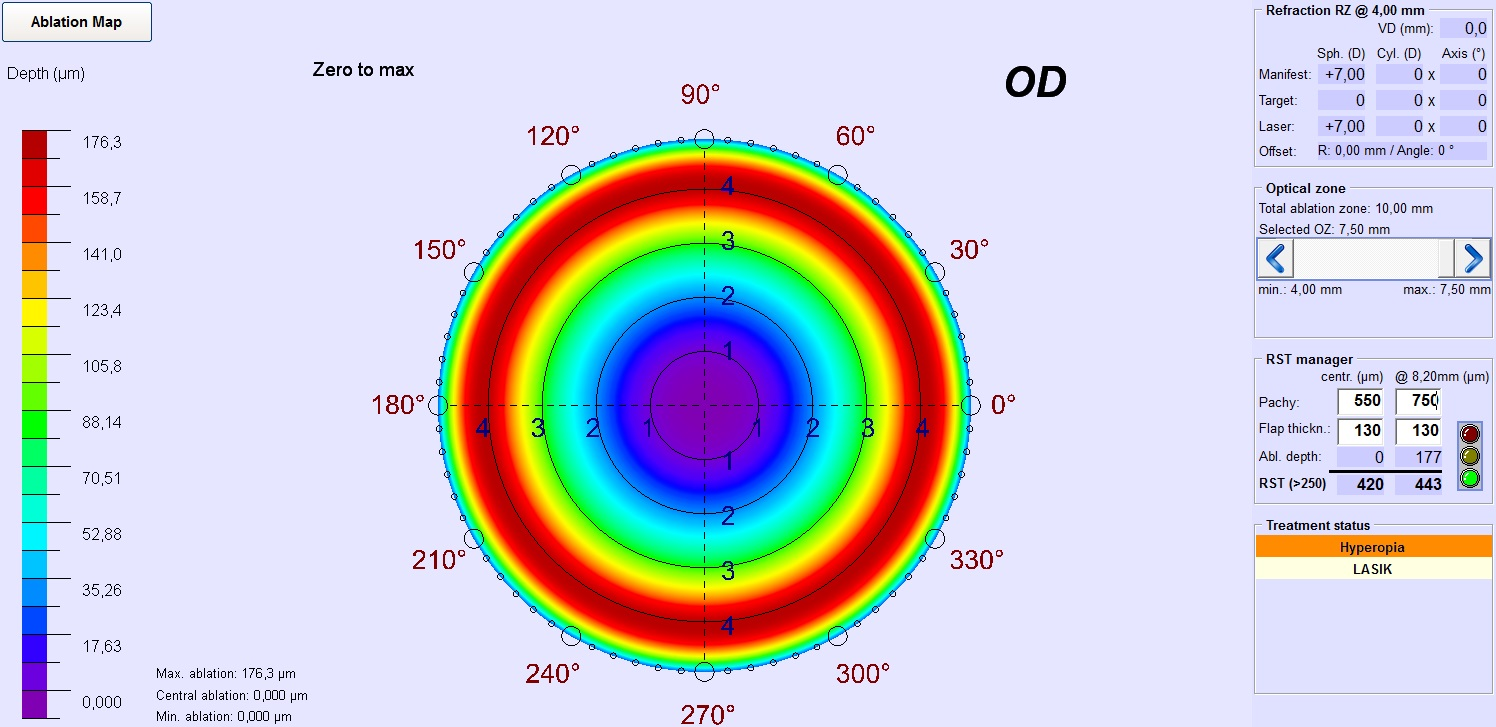
The SCHWIND AMARIS enables hyperopic correction up to +6D in LASIK and +5D in PRK (has approval for this range), but opens an “off-label” use accepting entries up to +8D (with user explicit acceptance). Several considerations must be accounted for, before setting a higher limit to the hyperopic refractive corrections. The natural shape of the cornea is an evolutionary optimum, being thinner at the center compared to the periphery. In any refractive treatment mode, the cornea must be manipulated in a way that the natural curvature and form of the cornea is retained as much as possible. Respecting this limit shall avoid making the cornea thinner in the periphery compared to the center. Considering an average corneal pachymetry (central ~550µm and peripheral ~700µm at 8mm diameter4; with its involved variations), and expressing the limit to retain the natural cornea form in diopters, the upper limit for hyperopic correction comes to be +7D. Interestingly, this upper limit is irrespective of the optical zone size and only relates to the center to optical edge variations in pachymetry. In our personal impression, this limit of +7D being imposed by center-to-periphery pachymetry, cannot be committed for a large population and is subject to inter-individual variability.
In addition, one must also consider the post-operative reepithelization and its associated risks, in treatment modes involving epithelial removal and regrowth. Reepithelization could render thinner epithelium over steeper areas of the cornea. Considering that the average keratometry in human eyes is 43.7D in vertical meridian and 42.7D in horizontal meridian, with a standard deviation of 2D5, 97 percentile of the human population has a natural keratometry of 48D in the vertical meridian6. Hence targeting a postoperative keratometry of 48D can definitely be considered safe. Taking 3 standard deviations to this average value, renders an extreme limit of 50D for post-operative target keratometry, beyond which the safety limits are surpassed6. These values result in a treatment limit of +7D in extreme situations and +5D with conservative measures. It must be noted that these values are based on statistical average of the human population, excluding the inter-individual differences among the population. LASIK may also have an effect on epithelial thickness with the epithelium being thinnest over the steepest part of the cornea. In some cases this may lead to “apical syndrome” where corneal scarring can occur and in very rare cases to diurnal variation in refraction and vision that is consistent with a diurnal fluctuation in epithelial thickness7.
Human eyes tend to have a natural spherical aberration of +0.1µm8. It has been evaluated using adaptive optics that the human eye is capable of comfortably tolerating up to 0.56µm of positive or negative spherical aberration at a 6mm diameter. This suggests that the human eye can safely tolerate up to -0.66µm of spherical aberration induced through hyperopic corrections9. Most modern laser systems induce slightly less than 0.1µm of negative spherical aberration per diopter of correction, again suggesting a similar upper limit for hyperopic correction, of approximately +7D.
Different treatment modes may also have different implications on the upper limit of hyperopic correction.
Surface ablation methods like PRK may be detrimental since epithelium may react more aggressively making the outcomes regress more. On the other hand, LASIK flaps are too small in extreme hyperopic corrections, since the exposed surface becomes larger from the cornea steepening introduced by the ablation profile. This has also shown to increase the risk for epithelial ingrowth10. Repositioning the LASIK flap after such a treatment may induce undercorrection since the flap cannot follow the deep and steep doughnut shape of the ablation, but also (vertical) coma, since the flap cannot cover the ablation completely. Considering these implications, for high hyperopic corrections extremely large flaps and optical zone sizes (fitting optical zones with large transition zones) must be targeted for LASIK treatments while large optical zones sizes must be targeted for surface ablation methods like PRK. A low curvature gradient along the optical and transition zone is considered to reduce regression11. Patients with high levels of hyperopia need to be warned that they may lose lines of CDVA following any correction for high hyperopia due to minification of the image on the retina compared to the spectacle image created on the retina. The same effect is seen with IOL’s correcting high levels of hyperopia.
References
1 Azar DT, Primack JD. Theoretical analysis of ablation depths and profiles in laser in situ keratomileusis for compound hyperopic and mixed astigmatism. J Cataract Refract Surg 2000;26:1123–36.
2 Llorente L, Barbero S, Merayo, Marcos S. Total and corneal optical aberrations induced by laser in situ keratomileusis for hyperopia. J Refract Surg. 2004;20(3):203-216.
3 Kohnen T, Mahmoud K, Buhren J. Comparison of corneal higher- order aberrations induced by myopic and hyperopic LASIK. Ophthalmology. 2005;112(10):1692.
4 Feizi S, Jafarinasab MR, Karimian F, Hasanpour H, Masudi A. Central and peripheral corneal thickness measurement in normal and keratoconic eyes using three corneal pachymeters. J Ophthalmic Vis Res. 2014 Jul-Sep;9(3):296-304. doi: 10.4103/ 2008-322X.143356.
5 Llorente L, Barbero S, Cano D, Dorronsoro C, Marcos S. Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations. J Vis. 2004 Apr 22;4(4):288-98.
6 Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness after hyperopic LASIK: three-dimensional display With Artemis very high-frequency digital ultrasound. J Refract Surg. 2010; 26(8):555-564.
7 Reinstein DZ, Gobbe M, Archer TJ, Carp GI. Mechanism for a Rare, Idiosyncratic Complication Following Hyperopic LASIK: Diurnal Shift in Refractive Error Due to Epithelial Thickness Profile Changes. J Refract Surg. 2016 Jun 1;32(6):364-71.
8 Thibos LN, Hong X, Bradley A, Cheng X. Statistical variation of aberration structure and image quality in a normal population of healthy eyes. J Opt Soc Am A Opt Image Sci Vis. 2002 Dec;19(12):2329-48.
9 Rocha KM, Vabre L, Harms F, Chateau N, Krueger RR. Effects of Zernike wavefront aberrations on visual acuity measured using electromagnetic adaptive optics technology. J Refract Surg. 2007 Nov;23(9):953-9.
10 Mohamed TA, Hoffman RS, Fine IH, Packer M. Postlaser assisted in situ keratomileusis epithelial ing-rowth and its relation to pretreatment refractive error. Cornea. 2011 May;30(5):550-2.
11 Vinciguerra P, Azzolini C, Vinciguerra R. Corneal curvature gradient determines corneal healing process and epithelial behavior. J Refract Surg. 2015 Apr;31(4):281-2. doi: 10.3928/1081597X20150319-08