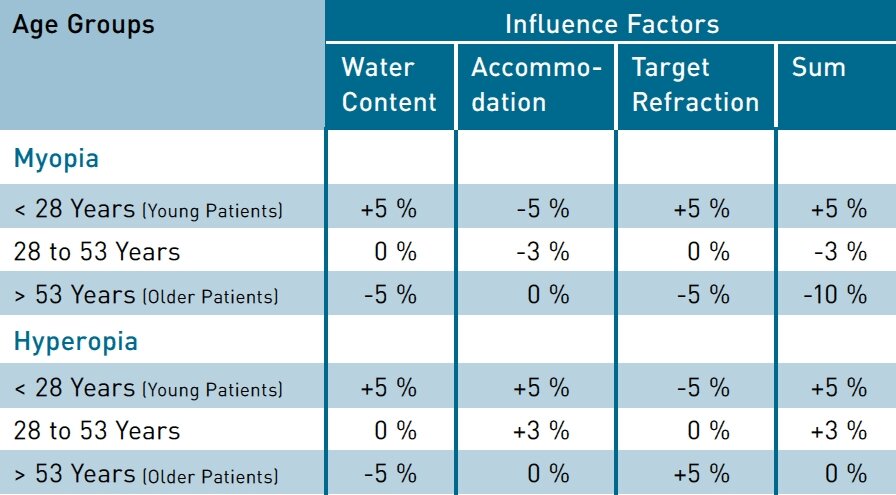
The SCHWIND AMARIS laser systems incorporate an age-based nomogram which considers water content of the cornea, over-/underrefraction through accommodation influences and the planned outcome (target refraction). Background: The water content of the cornea decreases as age increases1,2 – independent from the amount or type of refraction. The more water the cornea contains, the less efficient the ablation.3,4 This means that typically, with younger patients, the ablation per pulse is the least and becomes greater with increasing age. The ability to accommodate decreases with age 5,6,7 and it is also independent from the amount and type of refraction. This means that in age groups up to 53 years in case of myopia the measured refraction tends to be too high8, while respectively in case of hyperopia the measured refraction tends to be too low.
Younger patients are therefore more content with their quality of vision when the refractive outcome is slightly hyperopic. Satisfaction of older patients increases with a slightly myopic residual refraction because the ability to accommodate recedes. All of these influential factors are dynamically and progressively considered. The SCHWIND AMARIS scales the ablation profile corresponding to the age entered in the planning software.
Using all three influence factors, SCHWIND AMARIS incorporates the following age-based nomogram: In myopic cases, the AMARIS profiles include +5% over planning for young patients, -3% under planning for the age group 28 to 53 years and -10% under planning for older patients compared to the input value. In hyperopic cases, AMARIS profiles include +5% over planning for young patients, +3% over planning for the age group 28 to 53 years and neutral planning for older patients compared to the input value.
I recently evaluated the influence of age factors in a comprehensive study with 812 myopic eyes. The mean patient age was 38 years (between 18 and 61 years). All patients underwent an Aberration-Free LASIK treatment with the SCHWIND AMARIS and were observed up to one year postoperatively. The preoperative sphere ranged from -12.25 to -5.00 D, astigmatism up to 4.25 D was treated. Sphere and cylinder values were based on manifest refraction without nomogram compensation. All treatments used an optical zone basis of 6.0 to 6.8 mm. The total ablation zone was between 7.3 and 9.3 mm. In all cases, the treatment aimed to correct the visual defect and consequently to improve uncorrected distance vision – without inducing aberrations or reducing contrast sensitivity.
One year after treatment the mean global refractive deviation from the target refraction was +0.1 ±0.4 D for the spherical equivalent (SE) and 0.2 ±0.3 D for astigmatism. In 96% of treated eyes the spherical equivalent was within ±0.50 D of the planned outcome, in 91% the cylinder value was within 0.50 D of the planned outcome. Stability was achieved already one week after treatment.
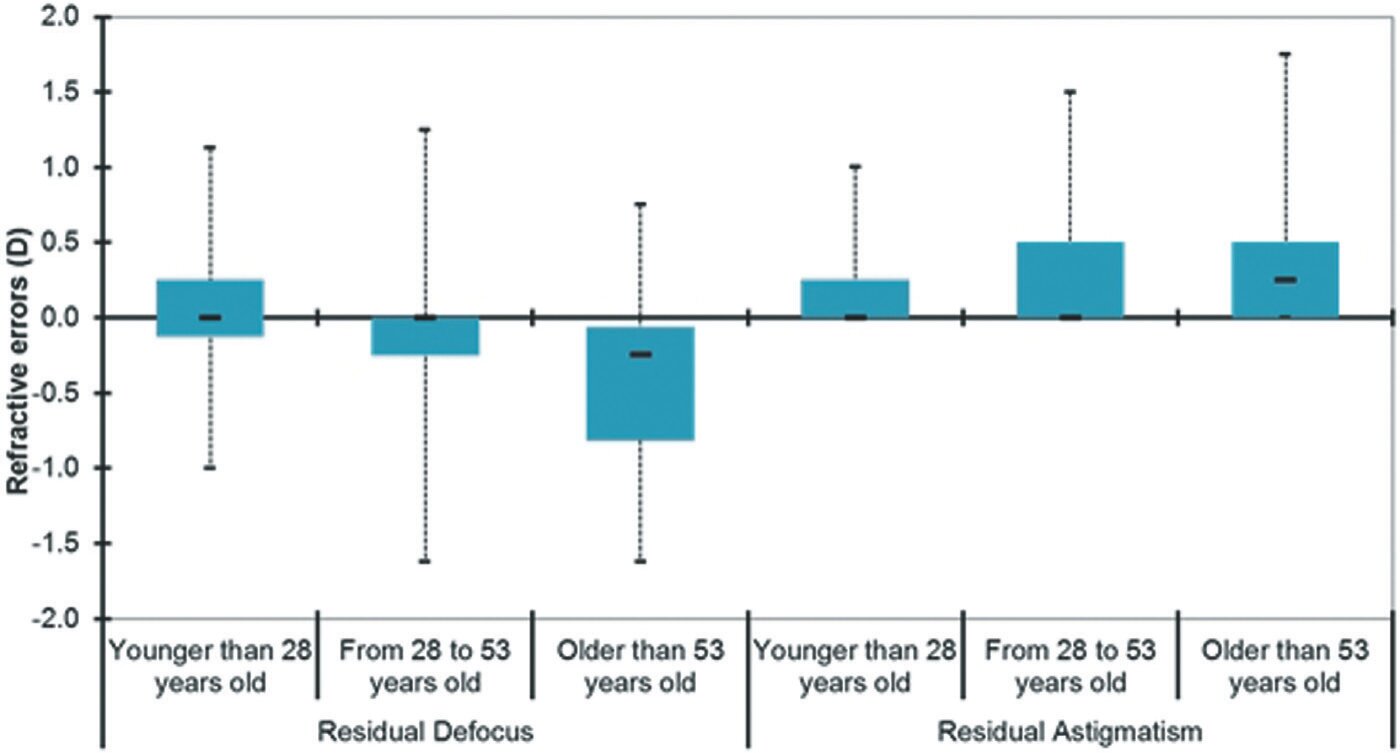
An analysis per age group showed the following residual refractions: In the group of young patients (<28 years) a spherical equivalent of +0.04 ±0.34 D and astigmatism of 0.19 ±0.28 was observed. The patient group between 28 and 53 years showed a sphere value of -0.07 ±0.34 D and astigmatism of 0.21 ±0.28 D. In the group of older patients (>53 years) a spherical equivalent of -0.40 ±0.51 D as well as astigmatism of 0.28 ±0.33 D was achieved. The outcomes confirm the accuracy of the age-based nomograms in the AMARIS profiles. The nomogram assures that the desired spherical refraction values are reached with no significant influence on cylinder values.
In conclusion: age, in this context meaning the time-related change of the condition of the cornea as well as of the internal eye, influences the clinical outcome. This occurs in dependence of the amount of the visual defect to be treated. The higher the planned refraction is, the greater the assumed deviation.
Residual refraction in the three age groups one year after treatment
As a consequence, age affects the outcomes on a percentage basis approximately proportional to the attempted correction and not on an offset basis. This means, for example, that a 70-year-old myopic patient would not automatically be measured with a residual sphere of +0.5 D or a 20-year-old myopic patient with -0.25 D. One would rather expect for the 70-year-old a spherical overcorrection of 10%, or for the 20-year-old an under-correction of 5%, if no age-based nomogram were to exist. The results further show that for each age group there is a different slope (angle) throughout the range of refractive power (steeper with high age) but not a constant (which would elevate or depreciate the line along the y axis). Thus, for every 10 years of age a change in planning of 3% should be considered, if no age-based nomogram were to exist.
1 Amparo F, Patel S, Alió JL, Rodriguez-Prats JL, Moreno LJ. Relationship Between Patient Age and Refractive Index of the Corneal Stroma During Refractive Surgery Assisted by Femtosecond Laser Flap Creation. Cornea. 2012 Feb 13. [Epub ahead of print]
2 Patel S, Alió JL, Amparo F, Rodriguez-Prats JL. The influence of age on the refractive index of the human corneal stroma resected using a mechanical micro-keratome. Cornea. 2011 Dec; 30(12):1353-7.
3 Kim WS, Jo JM. Corneal hydration affects ablation during laser in situ keratomileusis surgery. Cornea. 2001 May;20(4):394.
4 Dougherty PJ, Wellish KL, Maloney RK. Excimer laser ablation rate and corneal hydration. Am J Ophthalmol. 1994 Aug 15; 118(2):169-76.
5 Strenk SA, Strenk LM, Koretz JF. The mechanism of presbyopia. Prog Retin Eye Res. 2005 May;24(3):379-93. Epub 2004 Dec 19.
6 Atchison DA. Accommodation and presbyopia. Ophthalmic Physiol Opt. 1995 Jul;15(4):255-72.
7 Cervino A, Hosking SL, Rai GK, Naroo SA, Gilmartin B. Wavefront analyzers induce instrument myopia. J Refract Surg. 2006 Oct;22(8):795-803.
8 Thibos LN. Unresolved issues in the prediction of subjective refraction from wavefront aberration maps. J Refract Surg. 2004 Sep-Oct;20(5):S533-6. Review